Share Twitter Facebook Email Copy URL
Health and human rights are inextricably intertwined. Without the right papers, people may be denied government health services. They may be forced to pay for more expensive private doctors and clinics, or have to do without healthcare altogether. As a result, they tend to be less healthy than the general population. That is bad for everyone: sick people are less productive, and society has to pick up the bill.
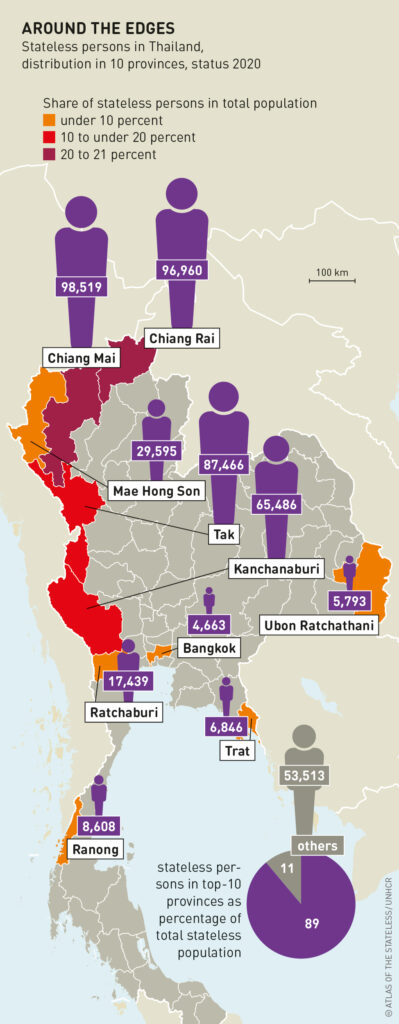
Thailand is home to around 500,000 stateless people, especially along the border with Myanmar. Many of them belong to ethnic minorities who have lived in the country for generations. As a result of various geographical, economic and educational barriers, the stateless individuals do not possess a birth-registration document indicating that they are Thai citizens.
In 2002, Thailand introduced universal health coverage for the whole population. Health protection is provided through three main public schemes: a civil-servant medical-benefit scheme for government employees and their dependants, a social security scheme for employees in the formal private sector, and a universal coverage scheme for everyone else.
The universal coverage scheme replaced a “Low Income Card Scheme”, which covered stateless people. But the Office of the Council of State of Thailand construed the 2002 National Health Act as meaning that the beneficiaries of the universal scheme must hold Thai nationality. That left stateless people without health coverage, forcing them to pay out-of-pocket for their healthcare. They made less use of health services; many were saddled with huge medical bills. Some hospitals went into debt because they provided subsidized services to stateless patients who were unable to pay their medical bills in full.
In 2010, after pressure from civil society, the Cabinet launched a new scheme called the Health Insurance for People with Citizenship Problems (HIPCP). This aimed to alleviate the financial difficulties of public hospitals in border areas and to increase access to healthcare among stateless people. The HIPCP provides similarly comprehensive benefits to the universal scheme: outpatient care, inpatient care, accident and emergency treatment, highcost care, and health promotion services.
health situation for refugees and stateless
people, but many problems remain
Stateless individuals must follow several steps to qualify for HIPCP insurance and access to healthcare services. They must first register with the Ministry of Interior, which confirms their nationality and assigns them a 13-digit identification number. They must then register with a health facility near their place of residence. The healthcare budget is set according to the number of people registered. Hospitals receive a fixed amount each year for each stateless person they have enrolled. Stateless patients who bypass their registered facility must cover the full cost of treatment, especially if they do not have an official referral letter.
Despite the comprehensive benefit package of free care, the HIPCP has failed to achieve its objectives of facilitating access to healthcare for its beneficiaries. This is due to operational problems at the local level, delays in the process of registering stateless people, insufficient collaboration between the ministries of public health and interior, and the lack of guidelines on budgeting as well as the scope of service provision for stateless patients.
Stateless children insured with the HIPCP use outpatient services 25 percent less often than their Thai counterparts insured with the universal scheme. But they use inpatient services 29 percent more, and are 34 percent more likely to stay in hospital. They are also more likely to fall ill with infectious diseases such as malaria, dengue, tuberculosis and diarrhoea. Overall, they seem to be in a poorer state of health.
In principle, there is no user fee at the point of service. But non-financial factors hinder stateless people from using outpatient services, especially in remote and rural areas. Primary healthcare posts in such areas are often hard to reach, which results in higher indirect costs: stateless people must on average travel over 30 minutes to get to the nearest primary healthcare post, and over two hours to reach the nearest hospital. The rainy season makes things worse.
While early diagnosis and treatment have cut the transmission of malaria in Thailand, most (79 percent) stateless people delay treatment or attempt to treat it themselves. In addition, many are infected with drug resistant strains of the disease. Low vaccination coverage and a lack of routine immunization add to the fact that relatively few stateless children are vaccinated, thus putting stateless children at greater risk of preventable diseases than their Thai counterparts.
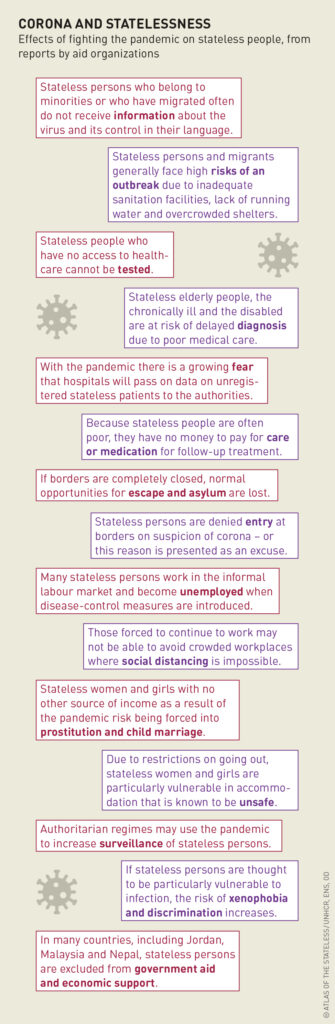
stateless persons are particularly hard-hit
by the effects of the Covid-19 pandemic
This contribution is licensed under the following copyright licence: CC-BY 4.0
The article was published in the Atlas of the Stateless in English, French, and German.